On Thursday, November 21, 2011, I attended the Mass Technology Leadership Council Breakfast Seminar, How Technology is Enabling Dynamic Community Care Teams. Rick Siegrist, the CIO at Press Ganey, began the morning with a discussion about integrated care. He explained that integrated care is not merely organizational legal integration or coordination of service. It is a patient-centered model that often involves coordination within and across multiple care teams as well as across community resources, especially in patients with serious or chronic illnesses.
Integrated care requires a continuity of relationships and familiarity with patients over time and must also take into account what happens to patients between visits with care providers. Providers must learn to look at the care they are providing from the patient’s viewpoint. At the same time, patients must share responsibility for and become engaged in their own care. To help with the integrated care model, Siegrist explains that providers are now able to mine with web for feelings in addition to facts using what he called “The New Science of Sentiment Analysis,” a process that analyzes customer opinions to extract feelings. Patient satisfaction surveys are a very meaningful database of information because when people are involved in a life and death situation or a trauma, their responses are likely to be more meaningful and honest because they have a strong personal connection to what occurred. Hospitals must take steps to respond to patient opinions and criticisms found in these surveys. If they don’t take action, patients with negative experiences will broadcast them on Facebook or blog about them, creating larger-scale negative publicity that providers and hospitals did not have to deal with in the past.
Siegrist concluded with an example of “low-tech” integrated care, explaining that Harvard Vanguard, Cleveland Clinic, Kaiser, Dartmouth and the VA have begun to offer shared medical visits for patients. Under this model, eight to 12 patients, all of whom sign privacy agreements, gather with a doctor, a nurse, a behaviorist and a documenter for a 90-minute appointment. Patients (who may or may not have similar medical conditions) take turns being examined and all are present for questions and explanations by the provider. The documenter records the entire appointment. These shared medical visits improve access to care (patients might get an appointment with a sought-after provider next week instead of six months from now), encourage patient involvement (patients share information with each other about their conditions) and garner higher provider satisfaction ratings (because providers do not feel rushed to move on to the next appointment). Take a look at his presentation here.
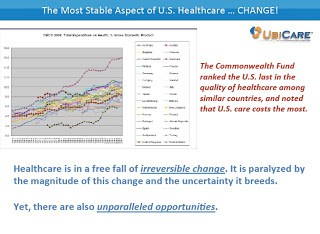
Betsy Weaver, CEO of TPR Media LLC, discussed her company’s recent launch of UbiCare (the name comes from the word, “ubiquitous”), a social media tool designed to enhance and streamline how healthcare connects with patients through Facebook, Twitter, text messaging and email. Weaver explained that US healthcare is facing irreversible change. Currently, quality of US healthcare is poor and costly, a combination that definitely needs to change. Healthcare’s solution must improve outcomes and create cost savings for patients and providers alike. She launched UbiCare because healthcare must be where patients are. A recent Pew Internet & American Life Project showed that 79% of all Americans are online, six of ten have wireless connections, small screens outnumber big screens and one of every three US adults has a smartphone. She explained that the only people who really do not use the Internet are those over 70 years old without a high school education. Betsy’s presentation is available here.
Ken Accardi, the CTO of iGetBetter.com, described how his company’s software allows hospitals to put patient discharge plans online and track patient follow-up care more closely. It gives providers the ability to monitor patient pain levels and see whether they are taking prescribed medication.
Coming at the health care relationship from a different angle, Benjamin Bielak, CIO of Dovetail Health, said that his company’s goal is to keep hospital admissions down and keep patients at home by developing an emotional connection with them, thereby reducing the risks of higher costs and potential illness stemming from hospitalization. Dovetail providers conduct an initial two-hour appointment where they ask patients what their emotional goals are. If a patient’s goal is to attend his daughter’s wedding, Dovetail works with the patient to try to reduce hospital admissions, keep the patient healthy and ultimately, to make his goal a reality.
Kathy Duckett, Director of Clinical Programs at Partners Healthcare at Home, told the group that her agency makes 3,600 home visits to patients each day, for a total of over 400,000 per year. Because PHH is a certified home health agency, it must abide by federal guidelines and regulations and is limited to providing skilled nursing visits to homebound patients. Despite these limitations, PHH must begin to think outside the box and has launched that Telehealth program which provides remote monitoring of 250 patients who are not homebound, but are frequently hospitalized. This program empowers patients to be more involved with their own care.
Finally, Marie Maloney, CIO of Senior Whole Health, spoke of the difficulties her agency encounters providing care to Medicare/Medicaid eligible patients with an average age of 74, many of whom are not connected to the Internet. They have adopted a member-centric model that provides care at the level deemed most appropriate for the patient, either annually, every six months or twice monthly. Forging a relationship with these patients and their families, only 46% of whom are English speaking, is the “secret sauce” to engaging these frail, uneducated seniors. Senior Whole Health employees speak many languages and care providers often come from the culture or community in which they are working.
So what is a dynamic community care team? First and foremost, it must be focused on patient needs and must respect what the patient wants. It requires participation from all those who are involved with a patient-providers, the patient, family caregivers (to the extent the patient wants family members privy to health care information), home health aides, and care managers. Ideally, a dynamic community care team will have a centralized record keeping system, where all those involved with a patient’s care can share access to information on a real time basis.
But questions and issues remain with respect to the use of technology to enhance patient care real time. Some providers, for example, are concerned about the use of email. If a patient or caregiver emails a provider about a high blood sugar level, for example, and the provider is unable to respond immediately, is the provider liable if something happens to the patient?
There is also a debate about what information should be shared. Providers want information they can act on; information overload is not helpful. Perhaps most helpful would be an easy-to-use system that can adapt to provide information providers want, based upon the changing needs of the patient. Unfortunately, this kind of system takes time and money to build. For it to work effectively, patients and providers must also be convinced of its value. While we are waiting for a better system, providers must continue to try to provide more integrated care, keep things simple and forge an emotional connection with patients to keep them invested in their own care.
Sharon Patton
November 22, 2011